This post starts out with some old news (from a blog perspective) -- news that is a week old.
At an AM conference at
Evanston Hospital, the hospital at which I am currently rotating (by the way, thanks so much
Dr. Wes for linking to my website and getting me started on a blogging addiction!), a
New York Times article regarding off-the-charts rates of angioplasty in Elyira, OH was brought to my attention.
The numbers speak for themselves.

The rate of angioplasty in Elyria is
almost double the next closest rate (I can see the people in Lafayette, LA getting nervous...) .
This sounds off the charts. But by another measure, it is
half-way to Mars.
The distribution of angioplasty rates above follows the classic bell-shaped curve (in this case the bell is depicted as lying on it's side).
Bell-shaped curves are found all over nature, and describe how randomly distributed variables tend to cluster around a mean (or average). Another important property of bell curves is the standard deviation, or a how "wide" the bell is.
A low standard deviation means most of the numbers fall close to the mean number, a high standard deviation means more of a spread. In fact, for an ideal bell-shaped curve, about 68% of the values fall within one standard deviation of the mean. About 95% fall within two. 99.7% fall within three. 999,999 out of a million fall within five. All but
one in 384 billion fall within seven.
I just had to get in touch with my inner geek and crunch some numbers in Excel. All I had to work with was the above graph. I found that the mean rate of angioplasties in the country for Medicare enrollees is about 11/1000. I found that the standard deviation is about 3.9 angioplasties /1000 Medicare enrollees. This means that the catheterization rate in Elyria, Ohio is about (42-11)/3.9, or about
7.9 standard deviations above the mean!This is really off the charts, and
cannot be explained by chance.
Now it's interesting that in Elyria there is one dominant cardiology group. One explanation offered in the article is that angioplasty rates are so high because many patients that might get bypass surgery at other hospitals get angioplasties in Elyria. If that's true, then the bypass rate should be rock bottom, right? Right?
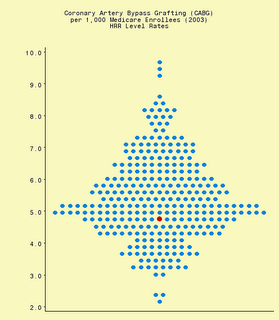
Someone also tipped me off to the
Dartmouth Health Atlas, a free online database of loads of healthcare information. I queried the database for a graph of the different bypass rates of all the 306 hospital regions in the country in 2003. I got:
The red dot is Elyria, pretty much smack dab in the middle. There goes that argument.
Who knows what the inevitable Medicare investigation will show, but I think it will show fraud. What motivates this? Is it greed on the part of the doctors? Is it the fact that the doctors and the patients don't see the cost of their actions?
Is this something that is widespread? Or is it just a few bad apples that fall very very fall from the main trunk of the bell-shaped tree?
What got me to post on this was an email I got forwarded from a friend of a friend who has just finished Cardiology fellowship, and is about a month into his new job as a general cardiologist in private practice. I know this person to be an excellent physician and an all-around good person. The email addresses the "rules" he has learned so far in private practice. I will post a part of it:
"...Cath EVERYONE. 3 of my first 4 caths were normals on patients who had a negative MPI [editor's note: a type of stress test that is pretty good] within the previous week. My group appreciates this. Funny thing, so do the patients' primary care docs, and so do the patients! Insurance companies can be dealt with ..."
Now, in editorial fairness, at the end of the email, this person also says "...OK, so I'm exaggerating, but the rules are clearly different..."
But I am left with the distinct impression that over-testing may be a widespread thing in Cardiology, which disheartens me a bit. I'd be interested to hear other's thoughts.